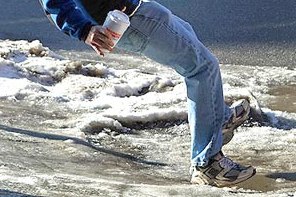
Afraid of falling this winter?
Now is the best time to work on prevention
Although it will (hopefully) be several months before the snow and ice start flying, September is a great month to start thinking about lowering your fall risk.
The good news is that it only takes 1-2 months to significantly improve your strength, flexibility, and balance, all of which work with other body systems to keep you steady.
Research has shown time and again that improvement in these areas has a significant impact on reducing the likelihood that an individual will fall.
When we address balance problems in physical therapy, we start by assessing our patient’s fall risk. There are several standardized tests that can be used for risk stratification and to set baselines.
A quick test that can be performed easily at home is to stand on 1 foot with your eyes open and hands on your hips. Make sure not to hook the lifted leg on the standing leg. If you’re unable to hold this for 10-15 seconds, you may be at an elevated risk of falling.
To learn more about falls and fall prevention from a physician’s perspective, I spoke to Dr. Maureen Doull.
Dr. Doull sees patients at Internal Medicine of Northern Michigan in Petoskey.
In your practice, at what age do you start to notice an increase in reported falls from your patients?
Doull: “Fall are very common in my practice and the incidence increases with age. Between 30-40 percent of people over 65 fall each year, and 50 percent of people over 80 fall each year. About 5-10 percent of falls result in a major injury such as fracture, head trauma, or major laceration. Unfortunately, most minor falls are never reported to physicians or other family members.”
Generally speaking, what are a few common contributing factors to falling?
Doull: “Risk factors for falls include: age, a past history of fall, lower extremity weakness, gait and balance problems, decreased visual acuity, female gender, orthostatic hypotension and use of psychotropic drugs such as pain medication and sleeping pills.
What are some things you recommend to your patients who have had a fall that resulted in an office visit?
Doull: “To determine the best intervention, we start by assessing their physical strength and balance with a few tests such as gait speed, raising from a chair (no hands allowed), or a timed up and go test. We encourage exercise or refer to physical therapy for strength and balance training.
“The provider will review the patient’s blood pressures and stop or discourage psychotropic drugs and encourage good nutrition. Depending on the circumstances, we may consider a home safety evaluation with recommendations such as grab bars, stair railings, non-slip rugs and bath mats, improved lighting, etc.”
If a person hasn’t fallen and wants to keep it that way, what can they can do to reduce their risk?
Doull: “Studies show benefit from group or home based exercise programs focused on muscle strengthening and balance, at least 3 hours/week. Exercise alone can decrease the rate of falls by 21 percent. It is important to avoid psychotropic drugs and remove home hazards. There is some evidence that Vitamin D-3 supplementation is beneficial if the patient is at risk for Vitamin D deficiency or has muscle weakness or balance problems.”
Jeff Samyn is a Physical Therapist, board certified Orthopedic Clinical Specialist, and Certified Strength and Conditioning Specialist at Northern Michigan Sports Medicine Center in Petoskey. He can be reached via e-mail at jsamyn@nmsportsmed.com. This information is not to be considered medical advice and is not intended to replace consultation with a qualified medical professional.