The 2018 football season is fast approaching and that means concussions are once again a hot topic on sports pages across the country. Unfortunately, concussion risk comes with the territory any time a sport involves contact between participants.
However, concussions are not just sustained by those engaged in tackling sports.
To understand the identification and prevention of concussions among athletes, I spoke with Dr. Todd Sheperd of Bayside Family and Sports Medicine in Petoskey and Lindsey Griffes, Athletic Trainer at Northern Michigan Sports Medicine Center who covers Petoskey High School athletics.
Both sports medicine professionals are frequently on the sidelines of high school football, hockey and basketball games throughout Northern Michigan during the school year.
Which sports or activities tend to have a higher frequency of concussions?
Dr. Todd Sheperd (TS): “Collision sports have the highest risk of concussion injuries. These sports include primarily football and hockey, both of which have rules that allow players to intentionally collide with the opponent. Even though non-contact sports (like soccer and basketball) have rules restricting intentional collisions, concussions still happen when players collide with each other or the ground.”
Are all concussions the same?
TS: “No, not all concussions are the same. Some have rapid recovery on the sideline and have very few lingering effects, while others can have symptoms which last for weeks or months and can interfere with both school and sports participation and performance.”
How do you recognize a concussion on the field?
Lindsey Griffes (LG): “The most obvious sign is observing an athlete take a hit to the head. Physical signs of a concussion may include the athlete appearing dazed or confused, mood or behavior changes that are out of character for the athlete, or tripping/stumbling. Cognitive signs including impaired response time to questions about time of day or the date, slowed or abnormal speech patterns, or not being able to recall events right before the injury are also indicators.”
What symptoms might a person with a concussion report?
LG: “Headache, dizziness, fatigue, sensitivity to light and sounds, vision problems, finding it difficult to focus or concentrate, feeling “in a fog” or “not right”, or general confusion.”
What kind of sideline testing do you perform to determine the severity of the concussion?
LG: “The tests which determine the severity of injury varies with each athlete. Generally we start by assessing the signs and symptoms mentioned above. I then assess cranial nerve function, as there are 12 cranial nerves which emerge from the brain and brainstem, all of which can be tested quickly on the sideline. If the athlete fails any portions of my assessment they are immediately removed from play and coaches and parents are informed during the game or practice. They may be referred to their health care provider for further evaluation and management.”
“If an athlete passes all of the cognitive tests and are symptom free, I will then perform a functional sideline test, the purpose of which is the engage the athlete in physical activity to see if any signs or symptoms manifest. Activities may include: running, sprinting, jumping, push-ups, or any other physical activity that gets the athlete moving without being placed back into the game or practice.”
What are the short and long term effects of a concussion?
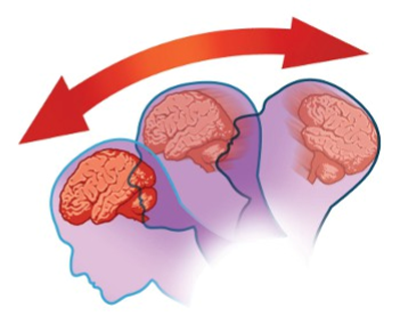
TS: “Short term effects include pain, changes in neurologic function (confusion, poor balance, lightheadedness etc.) as well as behavioral changes (mood, decreased concentration, irritability and poor sleep). Long term effects are more difficult to determine. Data suggests repetitive injuries to the brain can be associated with permanent impairment in memory (dementia), behavior (depression and other mood disorders) and movement disorders (sometimes similar to Parkinson’s disease).”
“There are multiple researchers currently investigating the long-term side effects related to concussion and other types of brain injuries (such as combat related injuries). One condition in particular has gained significant exposure in the press: Chronic Traumatic Encephalopathy (CTE). This condition appears to be related to repetitive head injuries and may develop symptoms involving behavioral changes as well as loss of memory and movement changes.”
“CTE was the subject of a recent major motion picture, and several former NFL players have had concerns regarding the development of this condition (although CTE is only clinically diagnosed after autopsy). There are many unknowns regarding how concussions may lead to CTE. Questions about factors such as genetic background, severity and number of head injuries as well as other risks including prior history of behavioral problems (depression, substance use) still need to be answered to allow sports medicine providers counsel their patients about the potential long term risks of repetitive head injuries.”
What can coaches, players, and parents due to prevent concussions?
TS: “The most consistent way to prevent concussions is to reduce the number of collisions and the energy involved in the impact. Despite the claims of many equipment manufacturers, adding additional layers of armor makes no significant change in the rates of concussions. Enforcing rules and changing player behavior, however, does reduce the risk of concussion in sports. For example, illegal checking in hockey and spearing in football often lead to concussions.”
LG: “The most effective action that can be taken is to follow and enforce the rules of the sport that are meant to ensure safe practices and games. These include avoiding hits to the head in football (targeting) and removing the athlete from play if headwear comes off or is not fitting properly.”
Jeff Samyn is a Physical Therapist, board certified Orthopedic Clinical Specialist, and Certified Strength and Conditioning Specialist at Northern Michigan Sports Medicine Center in Petoskey. He can be reached via e-mail at jsamyn@nmsportsmed.com. This information is not to be considered medical advice and is not intended to replace consultation with a qualified medical professional.